Adult Dermatology: Changes in Aging Skin
We won’t stay young forever, but that doesn’t mean our skin can’t continue to look its best. Adult skin changes as it ages, and some of these changes are more obvious than others. The trick to keeping your skin looking healthy and young for longer is prevention. Your Water’s Edge adult dermatologist can help you stall some of the side effects of age. Here are the five most-common effects of aging skin:
- Skin gets drier. Your skin produces fewer moisturizing oils as you age, so it’s important to protect your skin from losing moisture to wind, hot baths or the sun.
- Your skin begins to thin. Adult skin thins as you lose some of the fatty layer below your skin. Your skin cells regenerate more slowly and your collagen and elastin levels decrease as you age.
- Skin begins to sag. As your skin thins and you experience lymphatic drainage, gravity begins to pull on your skin. The decreasing levels of collagen and estrogen mean there is less structure for your skin as well.
- Age spots develop on exposed skin. Age spots are areas approximately the size of freckles. They are caused by melanin overproduction due to sun exposure.
- Wrinkles form and deepen. The most common causes of wrinkles are sun exposure, muscle and skin movement from facial expressions, slower skin cell regeneration and less collagen production. These are made more prominent by sagging skin.
Your skin is an indicator of your health, so keep it looking as good as you feel. Your adult dermatologist can treat dry and sagging skin, wrinkles and age spots. Make your appointment with a Water’s Edge dermatologist today and get serious medicine for your skin.
Treating Adult Acne
Acne is frequently considered a skin disorder of adolescents and teens. Unfortunately, acne can affect adults in their 20s, 30s and beyond. Many factors can contribute to the appearance of acne, including hormones, disorders of the hair follicles and infections. While there is no cure for acne, there are many effective ways to control and treat adult acne.
Adult acne can be divided in two groups of patients. The common acne in children can also occur in an adult, which is known as acne vulgaris. Another form of adult acne is known as acne rosacea. Acne rosacea is commonly recognized by the inflammation and redness of the face, but most often lacks the appearance of blackheads or open comedones.
Acne can be controlled with over-the-counter products as well as prescription medications. Establishing a skin care regimen with a dermatology provider can be very helpful in treating acne. Many treatments are available, including cleansers, topical treatment, oral antibiotic therapy, oral isotretinoin courses and even blue light therapy.
Starting with a mild antibacterial cleanser or benzoyl peroxide wash twice daily keeps the face and body clean and keeps oil to a minimum. Do not scrub the face and body clean as friction can increase the acne lesions.
Prescription treatments available for acne can be topical creams, gels or solutions. The topical medications can include one or more medications. Topical medications should be used consistently and as prescribed by your provider for best results. Topical treatments can be drying, so it is important to speak with your provider about adding a moisturizer or decreasing the frequency of use if this occurs.
Oral antibiotics can be used to treat acne and acne rosacea in adult patients. Oral antibiotic therapy can be given for short-term or long-term treatments, depending on the response to treatment and the medication prescribed by your provider. Low dose, long-term antibiotic therapy is available and effective for many patients.
Oral Isotretinoin is an option for severe acne. It was previously marketed under the name Accutane but is available now in generic forms. This particular medication is available if other oral medications have failed. Isotretinoin is closely monitored by a program called iPledge. Blood work is monitored each month by your provider. Two forms of birth control must be in place for female patients as this medication can cause birth defects if pregnancy occurs during the time period the medication is being administered. This medication is generally given for a course of four to six months.
The most important key to the management of acne is to be consistent with your use of medication. Consistency is important.
Finally, even acne prone skin needs sunscreen each day. Finding a sunscreen that is oil-free and non-comedogenic is important. Please visit a Water’s Edge office for Elta MD Shield, which is a zinc sunscreen that is lightweight, absorbs completely and is great for oily skin types.
References: Acne (n.d.) American Osteopathic College of Dermatology. Retrieved from www.aocd.org.
Top 5 Reasons to Consider Juvederm Voluma
Some signs of aging can begin to appear when women are in their mid-30s, such as cheeks losing volume or deepening under-eye circles. Fortunately, there are several ways to keep aging skin from detracting from your natural beauty, such as fillers like Juvederm Voluma. Here are the five top reasons why you should consider Juvederm Voluma when you decide to get a filler treatment.
- Restores fullness to your face by filling both fine and deep lines for a natural appearance.
- Diminishes any scars you may have accumulated over the years.
- Produces immediate results, meaning your face looks as youthful as you feel by the time you leave the office, and no downtime is required.
- Treatment is completed in one visit, so you don’t have to worry about scheduling multiple appointments.
- Results last for months, and when you combine certain fillers, your results can last between three months to a full year.
Juvederm is a smooth gel made from hyaluronic acid, which occurs in your skin naturally. Your Water’s Edge adult dermatologist can use the combination of Juvederm Voluma to smooth your skin and add volume and hydration. It is the latest facial filler option available and it is the only filler approved by the U.S. Food and Drug Administration.
Make an appointment with your Water’s Edge Dermatologist for a consultation about your filler treatment today. You can like us on Facebook to find more tips about skin care and our serious medicine for your skin.
Top Reasons to See a Professional for Mole Removal
Moles are removed for several reasons, whether medical or cosmetic. If you find your skin mole unattractive, it causes irritation from rubbing against clothing or your dermatologist suspects cancer, removing your mole, or moles, is an option.
There are several at-home and “natural” treatment options available, but these can cause complications if not performed correctly. Let’s talk about the top five reasons to have your skin mole treatment performed by your dermatologist.
- If your mole might be cancerous, or pre-cancerous, your dermatologist can help you begin treatments to prevent the spread of skin cancer. A dermatologist can have a sample of your mole tested when removing it, which cannot be done with at-home treatments.
- Your mole could grow back. Shaving or treating your skin mole at home may not completely remove the mole. If your mole does grow back, that is a possible sign of melanoma, for which you should be treated by a dermatologist.
- You could disfigure your skin by leaving scars. Especially on the face, it is important to have moles treated properly to avoid unnecessary scarring.
- The treatment site could get infected. A dermatologist can prevent infection from occurring by correctly preparing your skin for the mole treatment and by properly treating and closing the wound.
- Mole removal creams can leave pits in your skin. Some skin mole removal creams are corrosive and can cause damage to healthy skin if used incorrectly. If you want to try this method, it is recommended you discuss it with your dermatologist to minimize potential side effects.
Your Water’s Edge dermatologist can effectively remove your skin moles with one of two skin mole treatments: surgical excision or surgical shaving, both of which can be performed in-office. Make an appointment to discuss your skin mole treatment with your Water’s Edge dermatologist.
How to Give Yourself a Skin Mole Exam
You frequently hear dermatologists and skin cancer experts talk about the importance of regularly examining your skin, but do you know the best way to check yourself? Your skin moles should remain fairly constant, but here are the steps to find any new or changed moles.
Skin Mole Self-Examination:
- Start with your face, ears, scalp and neck. Use a hand mirror to see the back of your neck and a comb to part your hair to make this easier. Or, ask friend to help check your scalp.
- Stand in front of the mirror and look at the front and back of your body. Remember to raise your arms to look at your sides.
- Next, look at your hands and arms. Carefully examine your fingernails, palms and elbows, and look at your arms from all directions.
- Look at your legs from all angles using your mirror. Remember to check swimsuit areas for moles as well.
- Sit down and examine the bottoms and tops of your feet, your toenails and the spaces between your toes.
- Finally, take notes about your skin’s appearance and mark the dates of your skin mole exam. This will help you identify changes in your moles in the future.
Most of the moles you find likely developed when you were young, and you will continue developing skin moles until the age of 40. Most moles are harmless, but checking your skin regularly will help you track any changes and alert you to seek mole treatment if necessary.
If you find any suspicious or new moles, make an appointment with your Water’s Edge dermatologist to learn if you need skin mole treatment.
Botox®: Banishing More than Your Crow’s Feet
Botox Cosmetic is a simple treatment used to block nerve impulses to injected muscles to relax facial muscles and improve the look of wrinkles.
Here are some of the top reasons to talk to your Water’s Edge cosmetic dermatologist about Botox:
- Results are noticeable within days
- Recovery time is unnecessary
- It is a simple, nonsurgical procedure
- It relaxes your targeted muscles to smooth existing wrinkles and prevent new wrinkles
- Results last from three to 12 months
- Side effects, such as bruising or soreness, are minimal and uncommon
Your skin will age as you do and as you expose it to sun and environmental factors, but you can still look as young as you feel. Ask your Water’s Edge cosmetic dermatologist about whether Botox® is an option for you.
Water's Edge Dermatology: We’ve got serious medicine for your skin.
Skin Cancer Screenings for Skin Cancer Month
According to the American Cancer Society, skin cancer accounts for nearly half of all cancers in the United States, with one in five people having some form of skin cancer. Melanoma, the most serious type of skin cancer, will account for more than 76,600 cases of skin cancer in 2013, resulting in roughly 9,000 deaths annually.
“It’s so unfortunate when a patient waits too long to be screened and melanoma is found way too late, as it’s very treatable if found early,” says Justin Platzer, M.D., a board-certified dermatologist and Mohs skin cancer surgeon at Water’s Edge Dermatology.
Darlene Moore of West Palm Beach, Fla., echoes Dr. Platzer’s sentiment of the importance of diagnosing melanoma early. During a regular skin cancer screening at Water’s Edge Dermatology, Shanna Stone, ARNP, saw a few areas of concern on Ms. Moore’s ear and arm and took biopsies. Ms. Moore was diagnosed with Stage 1 melanoma on her arm and basal cell carcinoma on her ear.
“The basal cell, frankly, I wasn’t as concerned about,” says Ms. Moore. “Dr. Platzer reassured me that Mohs surgery was very effective for basal cell carcinoma and he was able to get it all. But I was really concerned about melanoma, because my brother-in-law died of melanoma.”
Surgery is the best way to remove early melanomas, with later stages usually requiring more extensive treatment, such as radiation and chemotherapy. Mohs surgery saves the greatest amount of healthy tissue, appears to reduce the rate of local recurrence and has the highest overall cure rate — about 94 percent to 99 percent — of any treatment for squamous cell carcinoma. And generally, Mohs surgery is 98 percent or better for basal cell carcinoma, according to the Skin Cancer Foundation.
“As the old saying goes, ‘An ounce of prevention is worth a pound of cure,’” says Dr. Platzer. “Say no to tanning beds and always wear sunscreen. And, if you live in sunny Florida, it is critical to have regular skin cancer screenings — and there’s no better time than this month, Skin Cancer Month.”
Many of Water’s Edge Dermatology clinics are open Saturdays and late during the workweek. To make an appointment, visit www.WeDerm.com and fill out the online appointment form, email info@WeDerm.com or call (561) 694-9493 for more information.
Skin Cancer Prevention Tips for Skin Cancer Awareness Month
May is Skin Cancer Awareness Month, and Water’s Edge Dermatology recommends the following skin cancer prevention tips to have fun in the sun and reduce risk for skin cancer at the same time:
- Generously and regularly apply water-resistant sunscreen that has a sun protection factor (SPF) of 30 or more. Make sure the sunscreen is labeled as “broad-spectrum,” indicating it protects against ultraviolet A (UVA) and ultraviolet B (UVB) rays. Reapply sunscreen every two hours and after swimming or sweating—and use it year-round.
- Use extra caution when taking sun-sensitizing medications or are near water, snow and sand. Some over-the-counter medications, such as ibuprofen, and prescription drugs, such as antibiotics, can make your skin more sensitive to sunlight. Water, snow and sand can reflect and/or intensify sun rays, making it easier to burn.
- Wear protective clothing, including long-sleeved shirts and pants, a wide-brimmed hat that provides more coverage than a baseball hat and UVA/UVB protective sunglasses.
- Seek shade during the middle of the day, between 10 a.m. and 4 p.m., when the sun’s rays are strongest, and try to schedule outdoor activities for other times of the day—even when it is cloudy.
- Say no to tanning beds. Ultraviolet light from tanning beds can cause skin cancer. New self-tanning lotions and spray booths provide a tan without the risk of cancer.
- Check your entire body routinely and report skin changes to your dermatologist. New growths, changes in existing moles or bleeding on the skin, require an immediate appointment with a dermatologist. Skin cancer is very treatable when caught early.
“As the old saying goes, ‘An ounce of prevention is worth a pound of cure,’” says Dr. Platzer. “Say no to tanning beds and always wear sunscreen. And, if you live in sunny Florida, it is critical to have regular skin cancer screenings—and there’s no better time than in May, skin cancer awareness month.”
When to See a Dermatologist for a Mole
Skin Moles are common. Almost everyone has a few, and some people develop hundreds. And melanoma, the deadliest type of skin cancer, can develop in or near moles.
Don’t get frightened—most skin moles are not melanoma. So how do you know when to see a dermatologist for your moles? It’s easy; just keep in mind your ABCs.
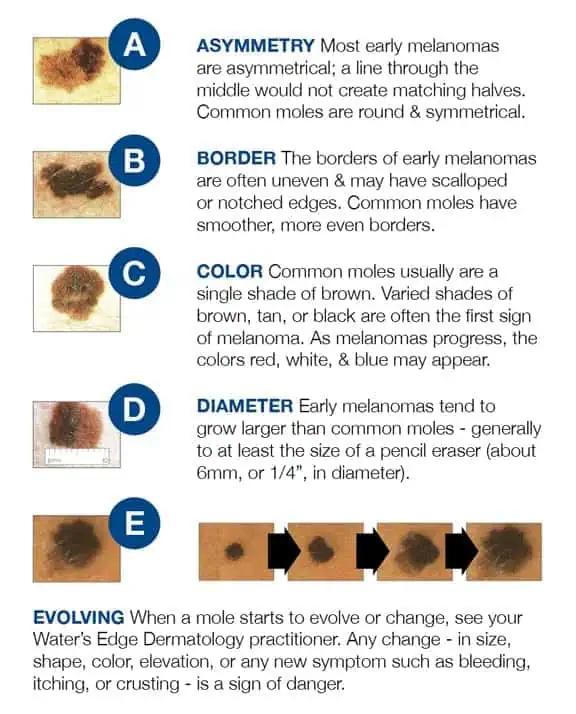
A stands for ASYMMETRY: If one half of the mole is unlike the other half, have it looked at.
B stands for BORDER: If your mole has an irregular, scalloped or poorly defined border, it could be an early melanoma. Only a biopsy can provide conclusive results.
C stands for COLOR: If a mole’s color varies from one area to another, or if it turns shades of tan, brown and black (opposed to brown, which is normal), call your dermatologist.
D stands for DIAMETER: Melanomas are usually greater than 6mm (the size of a pencil eraser) when diagnosed, but they can be smaller. If a mole is large, have it examined and stay very aware of changes or growth.
E stands for EVOLVING: A mole or skin lesion that looks different from the rest or is changing in size, shape or color could be a sign of early skin cancer.
If you have a mole that shows any of these signs, be sure to schedule an appointment with a Water’s Edge Dermatology provider today. If something doesn’t seem right, or keeps grabbing your attention, come see us.
When it Comes to Staph Infections, Prevention is the Key
Different varieties of Staphylococcus aureus bacteria, commonly called "staph," exist. “Staph infections” are common and a term I remember hearing since I was a child; so this is not something new. Staph bacteria are normally found on the skin and in the nose of about one-third of the population. The bacteria are generally harmless unless they enter the body through a cut or other wound, and even then they usually cause only minor skin problems in healthy people. However, Methicillin-Resistant Staphylococcus Aureus (MRSA) is different. MRSA infections are caused by a strain of staph bacteria that's become resistant to the antibiotics commonly used to treat ordinary staph infections.
Most MRSA infections occur in people with questionable immune function who have been in hospitals or other healthcare settings, such as nursing homes and dialysis centers. When it occurs in these settings, it's known as healthcare-associated MRSA (HA-MRSA). HA-MRSA infections typically are associated with invasive procedures or devices, such as surgeries, intravenous tubing or artificial joints.
Another type of MRSA infection occurs in the wider community — among healthy people. This form, community-associated MRSA (CA-MRSA), often begins as a painful skin boil. It's spread by skin-to-skin contact. At-risk populations include groups such as high school wrestlers, child care workers and people who live in crowded conditions.
Staph skin infections, including MRSA, generally start as small red bumps that resemble pimples or boils. It is not uncommon for the patient to suspect a spider bite. These can quickly turn into deep, painful abscesses that require surgical draining. In most situations, the bacteria remain confined to the skin. But in the case of the HA-MRSA, they can also burrow deep into the body, causing potentially life-threatening infections in bones, joints, surgical wounds, the bloodstream, heart valves and lungs.
Antibiotic Resistance:
MRSA is the result of decades of unnecessary antibiotic use. For years, antibiotics have been prescribed for colds, flu and other viral infections that don't respond to these drugs. Even when antibiotics are used appropriately, they contribute to the rise of drug-resistant bacteria in part because they don't destroy every germ they target. In addition, patients who do not take their entire course of antibiotics also play a role in the emergence of these resistant strains. Bacteria live on an evolutionary fast track, so germs that survive treatment with one antibiotic soon learn to resist others.
Because hospital and community strains of MRSA generally occur in different settings, the risk factors for the two strains differ.
Risk factors for HA-MRSA:
- Being hospitalized. MRSA remains a concern in hospitals, where it can attack those most vulnerable — older adults and people with weakened immune systems.
- Having an invasive medical device. Medical tubing — such as intravenous lines or urinary catheters — can provide a pathway for MRSA to travel into your body.
- Residing in a long-term care facility. MRSA is prevalent in nursing homes. Carriers of MRSA have the ability to spread it, even if they're not sick themselves.
Risk factors for CA-MRSA:
- Participating in contact sports. MRSA can spread easily through cuts and abrasions and skin-to-skin contact.
- Living in crowded or unsanitary conditions. Outbreaks of MRSA have occurred in military training camps, child care centers and jails.
- Men having sex with men. Homosexual men have a higher risk of developing MRSA infections.
When to see a Healthcare Professional:
Keep an eye on minor skin problems — pimples, insect bites, cuts and scrapes — especially in children. If wounds become infected, seek medical care. Do not attempt to treat an MRSA infection yourself. You could worsen it or spread it to others.
What You Can Do:
Create a list that includes:
- Detailed descriptions of your symptoms
- Information about medical problems you've had
- Information about the medical problems of your parents or siblings
- All the medications and dietary supplements you take
- Questions you want to ask the doctor
What to Expect During Your Visit:
During your physical exam, your doctor will closely examine any skin lesions you may have. He or she might take a sample of tissue or liquid from the lesions for testing.
Both healthcare-associated and community-associated strains of MRSA still respond to certain antibiotics. In some cases, antibiotics may not be necessary. For example, your doctor, NP or PA may choose to drain a superficial abscess caused by MRSA rather than treat the infection with drugs.
Preventing HA-MRSA:
In the hospital, people who are infected or colonized with MRSA often are placed in isolation as a precaution to prevent the spread of MRSA. Visitors and healthcare workers caring for people in isolation may be required to wear protective garments and must follow strict hand hygiene procedures. Contaminated surfaces and laundry items should be properly disinfected.
Preventing CA-MRSA:
Wash your hands. Careful hand-washing remains your best defense against germs. Scrub hands briskly for at least 15 seconds, then dry them with a disposable towel and use another towel to turn off the faucet. Carry a small bottle of hand sanitizer for times when you don't have access to soap and water.
Keep wounds covered. Keep cuts and abrasions clean and covered with sterile, dry bandages until they heal. The pus from infected sores may contain MRSA, and keeping wounds covered will help keep the bacteria from spreading.
Keep personal items personal. Avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. MRSA spreads on contaminated objects as well as through direct contact.
Shower after athletic games or practices. Shower immediately after each game or practice. Use soap and water. Don't share towels.
Sanitize linens. If you have a cut or sore, wash towels and bed linens in a washing machine set to the hottest water setting (with added bleach, if possible) and dry them in a hot dryer. Wash gym and athletic clothes after each wearing.
Most patients have come to know and often fear the term MRSA. However, when these infections are encountered the general community, in patients who are otherwise healthy, there is little to fear. Your healthcare provider will know exactly how to manage your condition and you are sure to recover without complication. Even so, it is still good behavior to practice the sound preventive measures we discussed above.