Treatment Options for Eczema
If you or someone you know has eczema, you know it can be itchy, irritating and hard to manage. It often can feel like no matter what you do to get rid of it, the rash stays or keeps coming back.
Eczema often starts at a young age, with 10-20 percent of children diagnosed with the condition. While it can be lifelong, eczema tends to become less severe with age.
Unfortunately, there are not effective, easy, over-the-counter treatments for eczema. There are, however, tools dermatologists can use to appropriately diagnose and treat eczema.
Medical research continues to show that the most effective treatment plan involves treating the skin and making lifestyle changes.
Eczema Treatment Options
Your Water’s Edge Dermatology practitioner may recommend any number of combinations of the following options to manage your eczema:
- Corticosteroid or an immune-modifying medication, which can help reduce the inflammation and itch
- An antihistamine can improve eczema that’s triggered by allergies
- Antibiotics if there’s an infection, which is common
- Ultraviolet (UV) light therapy
Lifestyle Changes for Eczema
Talk to your Water’s Edge Dermatology practitioner before you implement any of these lifestyle changes:
- Frequently applying an appropriate moisturizer
- Avoiding certain clothing
- Using eczema-friendly bathing techniques
If you think you or a loved one has eczema, schedule an appointment to have your condition properly diagnosed and to begin the path toward relief.
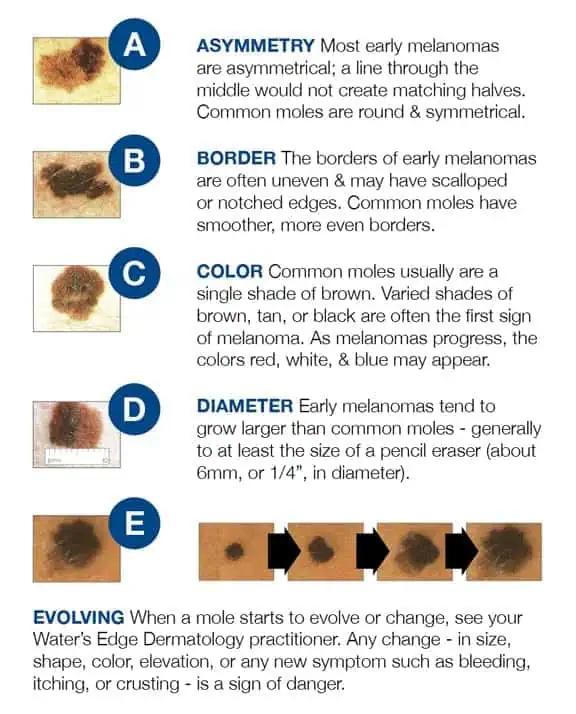
When to See a Dermatologist for a Mole
Skin Moles are common. Almost everyone has a few, and some people develop hundreds. And melanoma, the deadliest type of skin cancer, can develop in or near moles.
Don’t get frightened—most skin moles are not melanoma. So how do you know when to see a dermatologist for your moles? It’s easy; just keep in mind your ABCs.
A stands for ASYMMETRY: If one half of the mole is unlike the other half, have it looked at.
B stands for BORDER: If your mole has an irregular, scalloped or poorly defined border, it could be an early melanoma. Only a biopsy can provide conclusive results.
C stands for COLOR: If a mole’s color varies from one area to another, or if it turns shades of tan, brown and black (opposed to brown, which is normal), call your dermatologist.
D stands for DIAMETER: Melanomas are usually greater than 6mm (the size of a pencil eraser) when diagnosed, but they can be smaller. If a mole is large, have it examined and stay very aware of changes or growth.
E stands for EVOLVING: A mole or skin lesion that looks different from the rest or is changing in size, shape or color could be a sign of early skin cancer.
If you have a mole that shows any of these signs, be sure to schedule an appointment with a Water’s Edge Dermatology provider today. If something doesn’t seem right, or keeps grabbing your attention, come see us.
When it Comes to Staph Infections, Prevention is the Key
Different varieties of Staphylococcus aureus bacteria, commonly called "staph," exist. “Staph infections” are common and a term I remember hearing since I was a child; so this is not something new. Staph bacteria are normally found on the skin and in the nose of about one-third of the population. The bacteria are generally harmless unless they enter the body through a cut or other wound, and even then they usually cause only minor skin problems in healthy people. However, Methicillin-Resistant Staphylococcus Aureus (MRSA) is different. MRSA infections are caused by a strain of staph bacteria that's become resistant to the antibiotics commonly used to treat ordinary staph infections.
Most MRSA infections occur in people with questionable immune function who have been in hospitals or other healthcare settings, such as nursing homes and dialysis centers. When it occurs in these settings, it's known as healthcare-associated MRSA (HA-MRSA). HA-MRSA infections typically are associated with invasive procedures or devices, such as surgeries, intravenous tubing or artificial joints.
Another type of MRSA infection occurs in the wider community — among healthy people. This form, community-associated MRSA (CA-MRSA), often begins as a painful skin boil. It's spread by skin-to-skin contact. At-risk populations include groups such as high school wrestlers, child care workers and people who live in crowded conditions.
Staph skin infections, including MRSA, generally start as small red bumps that resemble pimples or boils. It is not uncommon for the patient to suspect a spider bite. These can quickly turn into deep, painful abscesses that require surgical draining. In most situations, the bacteria remain confined to the skin. But in the case of the HA-MRSA, they can also burrow deep into the body, causing potentially life-threatening infections in bones, joints, surgical wounds, the bloodstream, heart valves and lungs.
Antibiotic Resistance:
MRSA is the result of decades of unnecessary antibiotic use. For years, antibiotics have been prescribed for colds, flu and other viral infections that don't respond to these drugs. Even when antibiotics are used appropriately, they contribute to the rise of drug-resistant bacteria in part because they don't destroy every germ they target. In addition, patients who do not take their entire course of antibiotics also play a role in the emergence of these resistant strains. Bacteria live on an evolutionary fast track, so germs that survive treatment with one antibiotic soon learn to resist others.
Because hospital and community strains of MRSA generally occur in different settings, the risk factors for the two strains differ.
Risk factors for HA-MRSA:
- Being hospitalized. MRSA remains a concern in hospitals, where it can attack those most vulnerable — older adults and people with weakened immune systems.
- Having an invasive medical device. Medical tubing — such as intravenous lines or urinary catheters — can provide a pathway for MRSA to travel into your body.
- Residing in a long-term care facility. MRSA is prevalent in nursing homes. Carriers of MRSA have the ability to spread it, even if they're not sick themselves.
Risk factors for CA-MRSA:
- Participating in contact sports. MRSA can spread easily through cuts and abrasions and skin-to-skin contact.
- Living in crowded or unsanitary conditions. Outbreaks of MRSA have occurred in military training camps, child care centers and jails.
- Men having sex with men. Homosexual men have a higher risk of developing MRSA infections.
When to see a Healthcare Professional:
Keep an eye on minor skin problems — pimples, insect bites, cuts and scrapes — especially in children. If wounds become infected, seek medical care. Do not attempt to treat an MRSA infection yourself. You could worsen it or spread it to others.
What You Can Do:
Create a list that includes:
- Detailed descriptions of your symptoms
- Information about medical problems you've had
- Information about the medical problems of your parents or siblings
- All the medications and dietary supplements you take
- Questions you want to ask the doctor
What to Expect During Your Visit:
During your physical exam, your doctor will closely examine any skin lesions you may have. He or she might take a sample of tissue or liquid from the lesions for testing.
Both healthcare-associated and community-associated strains of MRSA still respond to certain antibiotics. In some cases, antibiotics may not be necessary. For example, your doctor, NP or PA may choose to drain a superficial abscess caused by MRSA rather than treat the infection with drugs.
Preventing HA-MRSA:
In the hospital, people who are infected or colonized with MRSA often are placed in isolation as a precaution to prevent the spread of MRSA. Visitors and healthcare workers caring for people in isolation may be required to wear protective garments and must follow strict hand hygiene procedures. Contaminated surfaces and laundry items should be properly disinfected.
Preventing CA-MRSA:
Wash your hands. Careful hand-washing remains your best defense against germs. Scrub hands briskly for at least 15 seconds, then dry them with a disposable towel and use another towel to turn off the faucet. Carry a small bottle of hand sanitizer for times when you don't have access to soap and water.
Keep wounds covered. Keep cuts and abrasions clean and covered with sterile, dry bandages until they heal. The pus from infected sores may contain MRSA, and keeping wounds covered will help keep the bacteria from spreading.
Keep personal items personal. Avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. MRSA spreads on contaminated objects as well as through direct contact.
Shower after athletic games or practices. Shower immediately after each game or practice. Use soap and water. Don't share towels.
Sanitize linens. If you have a cut or sore, wash towels and bed linens in a washing machine set to the hottest water setting (with added bleach, if possible) and dry them in a hot dryer. Wash gym and athletic clothes after each wearing.
Most patients have come to know and often fear the term MRSA. However, when these infections are encountered the general community, in patients who are otherwise healthy, there is little to fear. Your healthcare provider will know exactly how to manage your condition and you are sure to recover without complication. Even so, it is still good behavior to practice the sound preventive measures we discussed above.
The Skinny on Tanning Beds and Skin Cancer Risk
As dermatology providers, we have often been asked the question from our patients as to the risks of indoor versus outdoor tanning.
Well, the answers have recently become clear and are alarming! The rise in skin cancer rates happen to coincide with the growth of indoor tanning, which was first introduced in the U.S. in the 1970s. Just one single indoor tanning session can increase users’ chances of developing the most serious form of skin cancer, melanoma, by 20%. Each additional session during the same year increases the risk almost another 2%.
These figures are based on a recent exhaustive analysis of 27 studies by the International Research Institute in Lyons, France. Essentially, people who tan indoors are 74% more likely to develop melanoma in their lifetime. Those who started tanning before age 35 have an even higher risk of 87%, of developing Melanoma. The majority of tanning beds patrons are girls and women ages 16 to 29. They display a high level of knowledge about the risks of UV exposure, but this awareness does not alter tanning behavior.
The number of melanoma cases has tripled in the past twenty years. In 2012, melanoma has affected an estimated 76,250 people, killing 9,180 in the U.S. alone. The British Medical Journal published a study linking more than 5% of all melanomas to tanning bed use.
Heredity can play a major role in melanoma, but the disease is often be triggered by intense, intermittent sun exposure. Fair-skinned people with light hair and eye color and those who have had sunburns or tend to burn easily are at increased risk of developing melanoma. So are those who have a family history of the disease or have ever themselves had a melanoma or other skin cancer. People with unusual-colored and large-sized moles are at a higher risk. In the earliest stages, melanoma is readily treatable. Left untreated, however, it can spread to vital organs and become life-threatening. Among patients with advanced disease, just 15% survive longer than 5 years.
Further studies have shown the role of indoor tanning on non-melanoma skin cancers. Close to 171,000 (or about 3%) of non-melanoma skin cancers diagnosed each year in the U.S. are attributed to indoor tanning. A single UV tanning session increases squamous cell skin cancers (SCC) by 67% and basal cell skin cancer (BCC) by 29%. Additionally, indoor tanners under the age of 25 double their risk of SCC and increase their risk of BCC by 40%.
Skin cancer prevention is optimally about sun protection. Nonetheless, secondary prevention involves early detection. An annual head to toe skin exam by a dermatology provider is recommended by the Skin Cancer Foundation, with a monthly self-examination. Familiarize yourself with suspicious appearing lesions, new or changing moles, spots, sores, lesions or growths. When patients are diagnosed and treated at an early stage of skin cancer, almost all make a full recovery.
Remember to wear sunscreen, apply 1 oz (2 TBS) to your entire body 30 minutes before going outside. Reapply every 2 hours or after swimming or excessive sweating.
Unfortunately, despite recent efforts to educate the public and limit young peoples’ access to indoor tanning facilities, sunbathing and indoor tanning have not significantly decreased. Thirty million Americans still visit indoor tanning salons, annually. Suntans and sunburns occur from overexposure to UV radiation, and both are signs of damage to skin cells. So, let’s get the word out there.
Learn more about skin cancer, or request a skin cancer screening at Water’s Edge Dermatology.
Sources
Publication of the Skin Cancer Foundation, Revised 2012
Robbins, Perry, M.D., The Numbers Add up:Just One Tanning Session Multiplies Skin Cancer Risk., Sun and Skin News, Winter 2012, Vol. 29, No.4
ReedK., BrewerJd Lohsce Cm, et al, Demierre MF, LazovichD, et al, Karagas MR, et al, Swerdlow AJ, Weinstock. Teen Tanners, The New Face of Melanoma, Skin Cancer Foundation Journal, Vol XXX, 2012, 34-37
Common Viruses of the Skin & What You Should Know
Common viruses of the skin include Molluscum Contagiosum, warts, and Herpes Simplex Virus Type 1 and 2. These viruses are common because they are contagious with skin to skin contact. Although most are only an annoyance, some do have the potential to cause harm to the person affected. Our goal at Water’s Edge Dermatology is to educate and alleviate any possible concerns of our patients.
Molluscum Contagiosum is a common skin condition, especially in children, that comes from the Poxvirus. The virus presents as small umbilicated blisters and is usually diagnosed by a trained eye but can be confirmed with a biopsy. Contagiosum is an adjective that well describes the condition because it is so contagious. Children have more skin-to-skin contact and a lower immunity than adults, explaining why it is more commonly seen at a younger age. There are treatments such as liquid nitrogen or Cantharone (a topical agent) that are often used if the condition is bothersome or spreading. Treatment is not necessary because Molluscum Contagiosum is not harmful and with time should go away on its own. This condition can be sexually transmitted, but more commonly is spread by touching or scratching the area. Helpful tips for prevention include: avoiding direct skin-to-skin contact, avoid sharing towels with someone who is infected, frequent hand washing and protecting the skin's barrier by keeping it well moisturized.
Warts are caused by a virus called the Human Papilloma Virus (HPV), which is easily transmitted. Warts are also more common is children because their immunity is lower than adults. Most often, warts are diagnosed by a trained eye but can also be confirmed by a biopsy. There are different types of warts including; common warts, flat warts, plantar (under the surface of the foot) warts, and genital warts. Treatment may be the same as for Molluscum Contagiosum and is also a condition that may resolve on its own. Warts are typically raised but can be flat as in the flat warts or on the plantar surface of the foot. If warts are found in the genital region, they are usually considered to be sexually transmitted. However, common warts can also be transferred to the genitalia. Warts can be eradicated with treatment but they can return. Women who have a partner diagnosed with genital warts are at a higher risk for cervical cancer and should have regular pap smears. Helpful tips for prevention include: frequent hand washing; avoiding skin-to-skin contact with affected areas; wearing shoes in locker rooms, water parks, public pools and public showers to protect the feet; and protecting the skins barrier by keeping it well moisturized.
Herpes Simplex Virus (HSV) has two types (I and II), that when active, present with blisters or sores that can be painful. Type I is the cold sore virus and is generally found on the face, and type II is the sexually transmitted virus that is typically found in the genital area. However, type I has been found in the genitalia and type II has been found in other parts of the body. Once exposed to the virus, it may lay dormant for a long period of time, or may be such a mild case making it difficult to identify the source of infection. Stress and sun exposure can activate the dormant virus. HSV is contagious during flares but can also be contagious when no lesions are present. HSV is most commonly diagnosed by a trained eye, but a viral culture or blood work can be taken to confirm the diagnosis. HSV is treatable but there is no cure. Symptoms that may indicate the virus is active include tingling, itching, tenderness or burning sensation in the affected area. The treatment is antiviral medications like acyclovir or valacyclovir. If the medication is taken at onset, the symptoms may be minimized and the duration may be shortened. The symptoms will go away on their own with no treatment but may take longer than with the medication. Tips for prevention include: avoiding skin to skin contact to the affected area of a person with known HSV and avoiding sharing drinks, towels, lip balms or other products that may come in contact with the affected area.
These are some of the most common viruses of the skin but certainly not all of them. The key is early diagnosis and prompt treatment for any condition. Proper hand washing may not prevent these conditions, but is the number one way to avoid spreading infections. If you have any questions, please fill free to contact any of our offices. We are happy to help you in any way we can.
Mohs Surgery for Skin Cancer Treatment
Skin cancer is the most common type of cancer in the United States. And skin cancer rates are increasing in all races across the country.
At Water’s Edge Dermatology, our specially trained providers perform Mohs Surgery to treat skin cancer. Mohs micrographic surgery is a specialized, highly effective technique for the removal of skin cancer that is practiced throughout the world.
Here’s what Water’s Edge Dermatology patients are saying about Mohs Surgery.
Mohs Surgery permits the immediate and complete microscopic examination of the removed cancerous tissue, so all “roots” and extensions of the cancer can be eliminated. Due to the methodical manner in which tissue is removed and examined, Mohs surgery has been recognized as the skin cancer treatment with the highest reported cure rate.
Talk to your Water’s Edge Dermatologist about Mohs Surgery, or schedule your appointment for a skin cancer screening today.
Learn more about the types of skin cancer and skin cancer treatments.
Sunscreen: Your questions answered
Water's Edge Dermatology providing skin cancer and sunscreen awareness to UPS drivers.
Vitamin D
Vitamin D supplementation has been a recent media topic as well as a frequent question posed by our patients. Why the sudden hysteria? Actually, the vitamin D controversy is nearly 100 years old. It began in the 1920’s, around the same time period as the Coco Chanel’s trendy “tanned is beautiful” message. People who were tan were perceived to look healthier. This ultimately led to the public opinion that sun exposure was beneficial to health. This belief was further reinforced by the discovery of vitamin D being the active component in cod liver and shown to prevent childhood rickets as well as UV radiation causing vitamin D synthesis.
Despite the suspicion of UV radiation as a human carcinogen existing in medical literature as far back as the 1890’s the quest for tan began. There is now overwhelming evidence that UV radiation is carcinogenic. Melanoma and Non-melanoma skin cancers have continued to increase at dramatic rates characterizing these cancers as nearly epidemic. Despite the overwhelming evidence of the development of these cancers, the political crusade of some to promote unprotected UV exposure in order to increase ones photosynthesis of vitamin D in the skin still continues.
The question here is not in the benefit of adequate serum vitamin D levels, but more so in the ways to obtain these levels. Experts from the American Academy of Dermatology have examined the research and report evidence suggesting adequate vitamin D levels can be obtained through dietary consumption or supplementation equally and interchangeably as metabolizing it cutaneously from unprotected sun exposure.
Please take the time to review the recent article of Vitamin D from the Mayo Clinic.
http://www.mayoclinic.com/health/vitamin-d/NS_patient-vitamind
Vitamin D Fact Sheet Provided by National Institute of Health
What is vitamin D and what does it do?
Vitamin D is a nutrient that helps almost every part of the body. Like calcium, it builds bones and teeth and keeps them strong.
How much vitamin D do I need?
It depends on your age. Here are the amounts people of different ages should get on average each day, listed in International Units (IU):
Birth to 12 months
400 IU
Children 1–13 years
600 IU
Teens 14–18 years
600 IU
Adults 19–70 years
600 IU
Adults 71 years and older
800 IU
Pregnant and breastfeeding teens and women
600 IU
What foods provide vitamin D?
Only a few foods naturally have vitamin D. The best source is fatty fish like salmon, tuna, and mackerel. Beef liver, cheese, egg yolks, and mushrooms provide smaller amounts. You might be able to get recommended amounts of vitamin D by eating a variety of foods with plenty of fortified milk and fatty fish.
Almost all milk in the United States is fortified with 400 IU of vitamin D per quart. Vitamin D is also added to some breakfast cereals and brands of orange juice, yogurt, margarine, and soy beverages (check the product labels).
Can I get vitamin D from the sun?
The skin makes vitamin D when exposed to sunlight. But when out in the sun for more than a few minutes, wear protective clothing and use sunscreen (with an SPF of 8 or more) to lower the risk of skin cancer.
If you avoid the sun or cover your body with sunscreen or clothing, make sure you get enough vitamin D from food or take a supplement. When you're indoors, sunlight on your skin coming through window glass is not strong enough to make vitamin D.
What kinds of vitamin D dietary supplements are available?
There are two forms: D2 and D3. Both raise vitamin D levels in the body.
Am I getting enough vitamin D?
People with dark skin, older adults, obese people, and people with some digestive disorders (like Crohn's disease or celiac disease) may not get enough vitamin D unless they make a special effort. Breastfed infants should be given a vitamin D supplement of 400 IU each day.
Vitamin D can be measured in the blood to learn whether your levels are too low, too high, or somewhere in between. It's not yet clear what levels of vitamin D in the blood are best for good health.
What happens if I don't get enough vitamin D?
Vitamin D deficiency causes rickets in children, where the bones become soft and bend. It is rare but sometimes occurs, especially in African American infants and children. In adults, vitamin D deficiency causes bone pain and muscle weakness. Adults who don't get enough vitamin D and calcium can develop weak and brittle bones (osteoporosis).
What are some important links between vitamin D and health?
Scientists are studying vitamin D to see how it affects health. Here are a few examples of what this research has shown.
Bone problems
As they get older, men and women can develop weak and fragile bones, a condition called osteoporosis. Supplements of both vitamin D and calcium can reduce the risk of bone loss and fractures in elderly people. Talk with your healthcare provider about vitamin D and calcium as part of a plan to prevent or treat osteoporosis as you age.
Cancer
Some studies have tried to find out whether getting more vitamin D can affect the chances of developing cancers of the colon, breast, prostate, pancreas, and other parts of the body. It's too early to say whether low levels of vitamin D affect one's risk of cancer.
Can vitamin D be harmful?
In healthy adults, and in pregnant and breastfeeding teens and women, vitamin D at doses up to 4,000 IU is safe. (The safe amount is 1,000 IU for infants in the first six months of life and goes up as you get older to 4,000 IU in children age 9-13 years.) When taken as a supplement at very high doses, vitamin D can cause nausea and vomiting, confusion, and serious heart problems. Vitamin D made in the body from sunlight does not rise to dangerous levels.
Does vitamin D interact with any medicines or dietary supplements?
Yes. For example, prednisone and some medicines taken to lose weight, lower cholesterol, or control epileptic seizures can raise the need for vitamin D.
Bottom line: Tell your doctor, pharmacist, and other health care providers about any dietary supplements and medicines you take. They can tell you if those dietary supplements might interact or interfere with your prescription or over-the-counter medicines or if the medicines might affect how your body uses vitamin D.
Where can I find out more about vitamin D?
Office of Dietary Supplements Health Professional Fact Sheet on Vitamin D
Office of Dietary Supplements Consumer Fact Sheet on Vitamin D
Vitamin D Content of Selected Foods Per Common Measure
For advice on buying dietary supplements, see the Office of Dietary Supplements Frequently Asked Questions
For information on the government's food guidance system, see MyPyramid and the Dietary Guidelines for Americans
Disclaimer
This fact sheet by the Office of Dietary Supplements provides information that should not take the place of medical advice. We encourage you to talk to your healthcare providers (doctor, registered dietitian, pharmacist, etc.) about your interest in, questions about, or use of dietary supplements and what may be best for your overall health.
http://ods.od.nih.gov/factsheets/VitaminD-QuickFacts
Don’t give up. You can live with Psoriasis.
As difficult as the physical symptoms of psoriasis can be, the effect on an individual has emotional and social effects that are even more challenging. Studies have shown that psoriasis can have the same impact on quality of life as congestive heart failure or diabetes. It can be demoralizing to live with skin that’s different, and embarrassing to have people stare at you – or even avoid you – as if you had something contagious.
Psoriasis is a chronic autoimmune disease that appears on the skin. It happens when skin cells quickly rise from below the surface of the skin and pile up before they have a chance to mature.
The good news is that people don’t have to let psoriasis affect their quality of life. At Water’s Edge Dermatology, our practitioners are trained and experienced in treating psoriasis. We all have experience in treating this chronic condition. While there’s no cure yet, there’s plenty we can do together to make the psoriasis patient’s quality of life more manageable.
If you are suffering from psoriasis, it’s important to know that you’re not alone. As many as 7.5 million Americans deal with the challenges of psoriasis. With today’s treatments, you can live the life you want. Evolving treatments can improve the symptoms of psoriasis or even send them into remission. With patience and persistence, psoriasis patients can get back the life they want.
One question patients always seem to ask is “How severe is my psoriasis?” One way to measure the severity is how much of the body is covered. Mild is less than 3% of the body is covered. Moderate is 3% to 10% and Severe is more than 10%. A patch of psoriasis the size of the palm of your hand is equal to about 1% of your body surface.
Psoriasis often appears between the ages of 15 and 35, but can affect people of all ages and races, men and women equally. After treatment, it will often clear up for months, only to start again. Up to 30% of those with psoriasis also eventually develop psoriatic arthritis, which causes stiffness and swelling in and around the joints.
Putting together a successful treatment plan for the psoriasis patient depends on several factors. First, your practitioner will consider the amount of your body surface covered by the disease. But even more important is the severity of the patient’s symptoms and how they affect the quality of life.
How the patient feels about having the disease is very personal. One person may not be troubled by patches of psoriasis that can be kept covered. Someone else who has small patches on an area clearly visible may feel very embarrassed and want to try a more aggressive treatment.
Psoriasis is a non-contagious common skin condition that causes rapid skin cell reproduction resulting, in red, dry patches of thickened skin.
Guttate Psoriais looks like small salmon-pink drops on the skin.
At Water’s Edge Dermatology, our practitioners work with patients to determine what the patient wants from treatment, how long the patient has had the disease and what treatments have already been tried. This information is factored into the patient’s lifestyle, overall health and severity of symptoms. The most important factor in treatment is to follow the treatment plan that is developed exactly.
Treatment is dependant on the severity of the disease. Topical drugs may be used in mild to moderate cases of psoriasis. These topical drugs may be medicated lotions, ointments, creams, gels or shampoos. Most require a prescription.
Phototherapy uses ultraviolet light to treat moderate to severe psoriasis. There are three types of phototherapy. Ultraviolet B (UVB) – The patient’s skin is exposed to UVB rays generated from a special lamp or laser. The exposure causes reactions in skin cells that decrease their overproduction and help clear up plaques. Psoralen and Ultraviolet A (PUVA) – The patient ingests, applies topically or bathes in a drug called psoralen, then undergoes UVA exposure. The combination of the drug and the ultraviolet light slows skin cell growth. Excimer laser – A controlled beam of UVB light targets only affected areas, reducing inflammation and fast-growing skin cells. This treatment is appropriate for patients with very localized, mild disease. Body-wide medications – Moderate or severe psoriasis that has resisted other types of treatment may be treated with medications that treat your entire system. These medications may be taken orally, injected or infused by IV. They include Acitretin, Cyclosporine, Methotrexate, Alefacept, Adalimumab, Etanercept, Golimumab, Infliximab and Ustekinumab.
Psoriasis of the scalp may have fine, dry, scaly skin or have heavily crusted plaque areas. Psoriasis may only involve the nails.
Alternative approaches include sun and water therapy – short exposure to daily sunlight and the addition of water-ocean, hot springs or hot tub-helps soften plaques. Meditation can encourage an improved immune system response. Yoga teaches meditation and controlled breathing, which reduce stress (a common trigger). Nonprescription topical treatments, including aloe vera, evening primrose oil and capscaicin have all proven effective in clinical trials.
Medical treatment will go a long way toward helping the psoriasis patient control the disease. Making lifestyle changes can also be helpful in easing skin discomfort and minimizing periodic flare-ups. Adequate sleep, eating a balanced diet, regular physical exercise and drinking plenty of water will keep stress levels down and the body in top condition to fight off infection.
Diseases of the skin, like psoriasis, are reasons why everyone should have an annual skin examination by a dermatologist. At Water’s Edge Dermatology, our practitioners are highly experienced in psoriasis and all diseases of the skin. If you have any questions about psoriasis or other questions relating to skin care, Email them to me below. And if you haven’t had a skin examination in the past year, call one of our convenient locations for an appointment.
What Every Floridian Must Know About Skin Cancer
If you're like most Floridians, you've taken advantage of our summer and spent a good deal of time outdoors playing golf, tennis, boating, fishing, or just walking our magnificent beaches. In Florida, we are fortunate to enjoy these activities year-round. However, all of that exposure to the sun is something of which to be mindful. Skin cancer in Florida is more common because of the intensity of the sun.
According to the American Cancer Society, more than a million Americans will be diagnosed with skin cancer this year. In my dermatology practice, I have noted the increased number of patients that we are seeing with skin cancer. That’s not surprising when you understand the risk factors for skin cancer.
Exposure to UV radiation that comes from the sun, sun lamps, tanning beds or tanning booths is a primary risk factor. A person’s risk of skin cancer is related to lifetime exposure to UV radiation. Most skin cancer appears after age 50, but the sun damages the skin from an early age. UV radiation affects everyone. That’s why an annual skin exam is so important.
The two most common types of skin cancer are basal cell cancer and squamous cell cancer. They usually form on the head, face, neck, hands and arms. But skin cancer can occur anywhere. Basal cell skin cancer grows slowly. Squamous cell skin cancer sometimes spreads to lymph nodes and organs inside the body. The third form of skin cancer, Melanoma, is generally the most serious form of skin cancer because it tends to spread (metastasize) throughout the body quickly.
The most common warning sign of skin cancer is a change in the appearance of the skin, such as a new growth or a sore that will not heal. Unexplained changes in the appearance of the skin lasting longer than two weeks should be evaluated by an experienced dermatologist. According to the National Cancer Institute, the cure rate for basal cell and squamous cell cancers could be 100% if they were brought to a dermatologist’s attention before they had a chance to spread. Because cumulative sun exposure is a primary risk factor, it’s very important for all of us to have an annual skin cancer exam. In that manner, we can compare changes in the patient’s skin, from year-to-year.
Checking your skin for new growths or changes is a good idea. You should report any changes to your dermatologist right away.
Often, the first sign of melanoma is a change in the size, shape color or feel of an existing mole. Melanoma may also appear as a new mole. It may be black, or "ugly looking."
Don’t use photos to try to diagnose your own skin cancer. They can’t take the place of a dermatologist's examination.
If you haven’t made an appointment for your summer-ending skin cancer exam, now is the time. Skin cancer is the most common form of cancer. The earlier it is diagnosed, the better the chance for cure.